When it comes to treating temporomandibular joint (TMJ) disorders, patience is often key, as severe damage takes time to heal. For many people, dealing with TMJ pain can be a long-term process that requires a comprehensive approach to treatment. A recent study has shown that approximately 11-12 million adults in the United States experience pain in the temporomandibular joint region. This prevalence highlights the importance of understanding why TMJ treatment can take a significant amount of time. And because TMJ disorders are so poorly understood, many patients just do not know where to seek treatment. They fumble around with different doctors, trying to figure out what is really going wrong and by the time they find the right doctor, there is often a lot of jaw damage.
Understanding TMJ Disorder
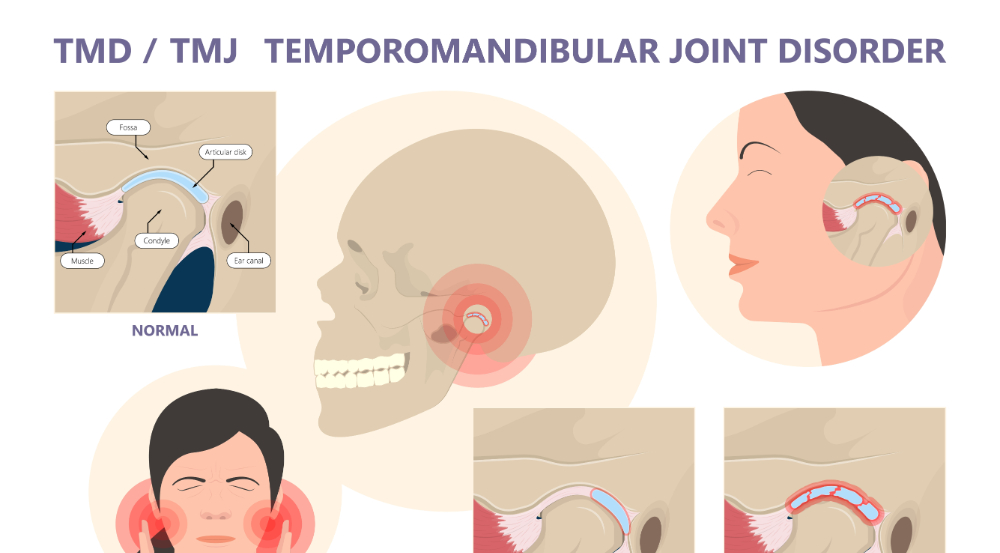
TMJ disorder is a complex condition that affects the jaw joint and surrounding muscles, causing pain, discomfort and difficulty in movement. These disorders are known to be more common in women, with data indicating that temporomandibular disorders are twice as prevalent in women than in men, particularly affecting women aged 35 to 44. (This was discussed in a previous blog.) Understanding the underlying causes and triggers of TMJ disorders is essential in designing an effective treatment plan and setting realistic expectations for recovery.
Initial Diagnosis and Assessment
In our practice, comprehensive initial diagnosis and assessment are crucial for effectively managing TMJ disorder. This process begins with a detailed medical history review, where patients discuss their symptoms, previous treatments and overall health. The next step is to conduct a physical examination, a complete head and neck palpation. The obvious focus is on the jaw joints and surrounding muscles to identify the pain points, clicking sounds or movement restrictions. Diagnostic tools used are imaging studies like CBCT X-rays and an MRI of the area. The CT scans are used to get a clearer view of the head, neck and jaw joint structure. This highlights any potential abnormalities. The MRI is used to see the function of the soft tissue. These diagnostic tools help gauge the severity of the TMJ disorder and pinpoint specific issues such as arthritis, dislocation, or muscle inflammation, compressed airway or eroding condyle. By gathering this detailed information, a tailored treatment plan can be created that addresses the unique needs and symptoms of each patient.
Custom Treatment Plans
Creating a custom treatment plan for TMJ disorder is crucial, as it addresses the individual needs and symptoms of each patient. This often involves a combination of therapies tailored specifically to the patient’s condition. Medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants or even low-dose antidepressants, may need to be prescribed (but not common) to manage pain and reduce inflammation. Physical therapy or TMJ massage therapy can play a significant role. This addition helps with relieving pain, strengthening the muscles and provides whys the patient can do exercises at home to help improve their health. These exercises are designed to improve the range of motion and alleviate discomfort.
In almost every case of TMJ disorder, appliance therapy is indicated. This involves wearing an orthotic device on the lower teeth to prevent the condyle (jawbone) from banging into the socket. An upper ALF appliance is most often used as well. This appliance helps to realign the cranium distortions. Together, the two devices take the pressure off the damaged discs and help the joint to heal.
Lifestyle modifications, including stress management techniques and dietary changes, are also integral to a comprehensive treatment plan. For patients with severe symptoms, oral appliances like orthotics are recommended to help reduce jaw strain and prevent teeth grinding. In more persistent cases, injections such as corticosteroids or Botox may be considered to relieve pain and improve function.
When non-surgical treatments are insufficient, more invasive procedures might be explored. However, the choice of treatment is always tailored to the specific needs of the patient, ensuring that all aspects of the disorder are addressed comprehensively. By employing a multifaceted approach, providers aim to offer the most effective relief and promote long-term healing.
Non-Surgical Treatments and Therapies
Non-surgical treatments and therapies are often the first line of defense against TMJ disorder. One effective method is manual therapy, which involves a physical therapist using hands-on techniques to stretch and manipulate the soft tissues around the joint. This type of therapy has been shown to improve function and relieve pain. Another promising treatment is prolotherapy, where a solution is injected into the TMJ area to provoke a healing response. This approach has shown promise, particularly for TMJ disorder involving dislocation or hypermobility of the joint.
Alternative therapies such as acupuncture and biofeedback may also be beneficial for some patients. Acupuncture involves the insertion of fine needles into specific points on the body to relieve pain and promote healing. Biofeedback teaches patients how to control muscle tension and stress through relaxation techniques and electronic monitoring.
In addition to the above therapies, a non-surgical option is available to manage TMJ disorder effectively. Oral appliances, like orthotics, are the best practice. The benefits are no surgery, helping to correct the problem but the downfall is it can take time. These appliances are custom-made to fit the patient’s mouth, offering better comfort and effectiveness. Adjustments are needed to keep progress moving forward. The frequency of these adjustments is based on each patient’s needs but typically eight to ten weeks to start. The goal is to have the displaced discs move back to the correct anatomical position. This in turn alleviates the symptoms and healing begins.
These non-surgical therapies provide a range of options for managing TMJ disorder, helping to alleviate symptoms and improve quality of life.
Surgical Interventions
For patients whose TMJ disorder does not respond to non-surgical treatments, surgical interventions may be necessary. These procedures can vary significantly in complexity and invasiveness. Arthrocentesis, a minimally invasive technique, involves inserting small needles into the joint to remove debris and inflammatory byproducts. Another less invasive option is arthroscopy, which uses a small camera and specialized instruments to treat the joint by realigning the TMJ disc (putting it back on top of the condyle) or removing the damaged perforated disc. For more severe cases, open-joint surgery (arthrotomy) may be required to repair or replace damaged joint components.
Choosing the right surgical intervention depends on various factors, including the severity of the disorder, the patient’s overall health and previous treatment outcomes. It is essential for patients to discuss the potential risks and benefits of each option with their provider to make an informed decision. Additionally, the expertise and experience of the surgical team play a crucial role in the success of the procedure. With advancements in surgical techniques and technology, the effectiveness and recovery times for TMJ surgeries continue to improve, offering hope for long-term relief.
Post-Treatment Rehabilitation
Now that the TMJ treatment is complete, it is vital to make sure the joints are supported for a successful finish. The focus is on restoring function and enhancing mobility. Other modalities are tailored to strengthen the jaw muscles, improve the range of motion and reduce pain. Procedures like laser therapy, massage therapy and gentle stretching exercises can aid tissue healing and reduce stiffness. Additionally, patients might be taught specific exercises to perform at home to maintain progress between therapy sessions if surgery is completed.
Lifestyle modifications are also essential during the finishing phase. Patients are often advised to adopt a soft diet initially to minimize jaw strain and gradually reintroduce more solid foods as they heal. Stress management techniques, such as mindfulness and relaxation exercises, can help prevent jaw clenching and teeth grinding, which can exacerbate TMJ symptoms. Regular follow-up appointments with your providers are necessary to monitor progress and adjust the rehabilitation plan as needed.
The orthotic and ALF appliances could continue to be used during this phase to ensure proper jaw alignment and prevent further strain. By adhering to a comprehensive rehabilitation plan, patients can optimize their recovery and achieve long-term relief from TMJ disorder.
Patient Commitment and Lifestyle Changes
Patient involvement is crucial for successful TMJ treatment. Incorporating healthy lifestyle changes can significantly enhance the effectiveness of various therapies. Eating a balanced diet that includes softer foods can reduce jaw strain. Stress management techniques such as meditation, yoga or deep breathing exercises can also alleviate symptoms by preventing jaw clenching and teeth grinding. Avoiding habits like chewing gum, biting nails or leaning on the chin can further minimize stress on the jaw joint. Regular use of prescribed oral appliances, such as splints or mouthguards, helps maintain proper jaw alignment and prevent additional strain. Consistent follow-up with healthcare providers ensures the treatment plan remains effective and adjustments are made as needed. Patient dedication to these changes plays a pivotal role in managing TMJ symptoms and promoting long-term recovery.
Ongoing Research and Future Outlook
Ongoing research in the field of TMJ disorders is paving the way for innovative treatments and enhanced patient outcomes. Scientists and medical professionals are continually exploring new approaches to understanding and managing these complex conditions. Recent studies have focused on the genetic and molecular factors contributing to TMJ disorder, which could lead to more personalized treatment options. Advanced imaging technologies are also being developed, allowing for more precise diagnosis and targeted interventions.
One promising area of research is the use of regenerative medicine techniques, such as stem cell therapy, to repair damaged tissues in the jaw joint. These approaches hold the potential to not only alleviate symptoms but also address the underlying causes of TMJ disorders. Additionally, the development of less invasive surgical techniques aims to reduce recovery times and improve the overall effectiveness of treatments.
Another exciting avenue is the integration of digital health technologies, including telemedicine and mobile health apps, to enhance patient monitoring and adherence to treatment plans. These tools can provide real-time feedback and support, making it easier for patients to manage their condition and communicate with their healthcare providers.
Moreover, interdisciplinary research efforts are exploring the connections between TMJ disorders and other health conditions, such as chronic pain syndromes and autoimmune diseases. By understanding these links, healthcare providers can develop more comprehensive and effective treatment strategies.
As our knowledge of TMJ disorders continues to expand, the future holds the promise of more effective and less invasive treatment options. Patients can look forward to improved quality of life and quicker recovery times, thanks to the ongoing advancements in research and technology.
If you need help with TMJ treatment in Falls Church, Virginia, Dr. Jeffrey Brown and our team at Sleep & TMJ Therapy invite you to call our office at 703-821-1103 to learn more or seek treatment.
