Experiencing jaw pain or discomfort can be alarming, especially if it interferes with your daily life. A common issue related to jaw pain is a perforated TMJ articular disc. The temporomandibular joint (TMJ) plays a crucial role in connecting your jaw to your skull, allowing for smooth movement. However, when the disc within this joint becomes perforated, it can lead to significant discomfort and potential complications. Understanding this condition is the first step toward effective management and relief.
Understanding the Temporomandibular Joint (TMJ)
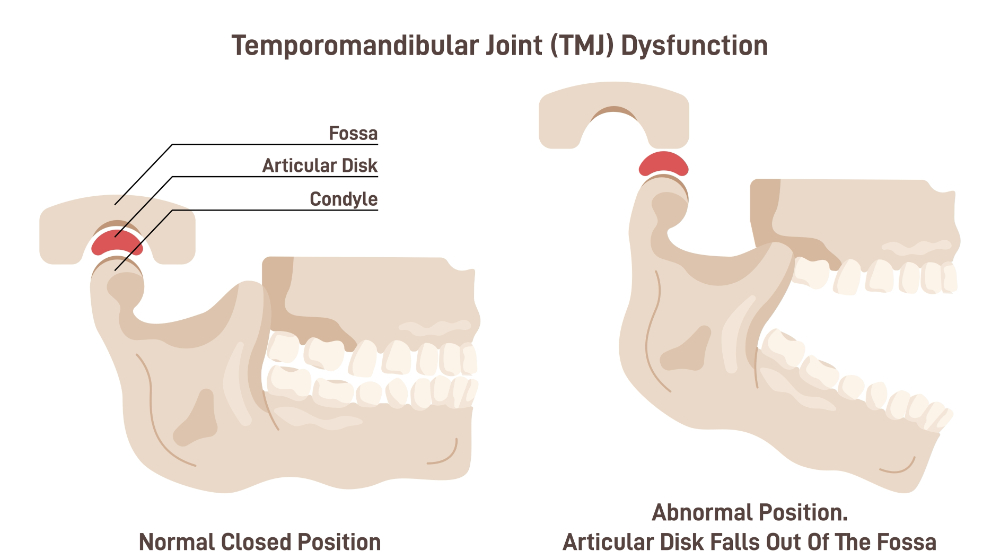
The temporomandibular joint (TMJ) is a vital and intricate structure in the human body. Situated on either side of your head, just in front of your ears, the TMJ functions as a sliding hinge, enabling various jaw movements such as opening, closing and lateral motion. This joint is essential for daily activities like chewing, speaking and yawning. Within the TMJ, a small, cartilage-based articular disc serves a crucial role in cushioning the joint, absorbing shocks, and ensuring smooth interactions between the jawbone and the skull. The disc’s integrity is vital for the proper functioning of the TMJ, as any damage can disrupt its role and lead to significant discomfort. When an articular disc is slipped or displaced off the condyle (top of the jawbone), this can cause significant pain in the head and neck region. A displaced disc is also associated with headaches, migraines, dystonia and even tremors.
What is TMJ Disc Perforation?
TMJ disc perforation is a condition where the articular disc within the temporomandibular joint develops a tear or hole. This issue disrupts the disc’s normal function of cushioning and stabilizing the joint, leading to misalignment and improper movement of the jaw. The compromised disc can no longer provide the necessary support, resulting in pain, inflammation and restricted jaw movement. Disc perforation represents a more advanced stage of TMJ disorder, requiring medical attention. Factors like chronic teeth grinding (bruxism), trauma or underlying arthritic conditions can contribute to the wear and tear of the disc, making it more susceptible to perforation. Early identification and intervention are essential to manage this condition effectively. A properly done MRI of the TM joints is the best way to analyze the problem and identify the perforated disc. However, getting that excellent imaging is quite difficult for some reason. Again, lack of awareness amongst the medical professionals makes dealing with TMJ disorder understandably difficult.
Causes and Risk Factors of TMJ Disc Perforation
Several factors can contribute to the development of a perforated TMJ disc. Chronic clenching or grinding of teeth, also known as bruxism, is a major contributor, as it places excessive stress on the temporomandibular joint. Trauma to the jaw, such as from an accident or a physical impact, can also result in disc perforation. Additionally, certain arthritic conditions, such as osteoarthritis or rheumatoid arthritis, can weaken the disc and make it more prone to tearing. Structural abnormalities of the jaw, either congenital or acquired, can also increase the risk. It is important to recognize these risk factors early to implement preventive measures and seek timely medical advice for effective management.
Symptoms of TMJ Articular Disc
Symptoms of a perforated TMJ articular disc can vary widely among individuals, making it essential to recognize the signs early. Persistent jaw pain is one of the most common symptoms, often exacerbated by activities like chewing, speaking or yawning. You might also notice clicking, popping or grating sounds when you move your jaw. These noises occur due to the misalignment and instability caused by the damaged disc. Another symptom to be aware of is difficulty opening or closing your mouth fully, sometimes referred to as jaw locking. This can be particularly alarming and uncomfortable. Swelling and tenderness around the temporomandibular joint are also frequently reported, adding to the overall discomfort. In some cases, individuals may experience headaches, earaches, fullness in the ears and even tinnitus (ringing, buzzing and hissing) as the TMJ is located near the ear canal. These symptoms can significantly impact daily activities, emphasizing the need for timely medical consultation.
Treatment Options for TMJ Disc Perforation
Treatment options for a perforated TMJ articular disc range from conservative approaches to surgical interventions, depending on the severity of the condition. Non-surgical treatments often serve as the initial step, aimed at alleviating symptoms and improving joint function. In almost all cases an orthotic is commonly recommended to reduce stress on the TMJ. The orthotic device is always placed on the lower teeth and must be worn 24 hours per day to reduce the loading effect on the joints.
In cases where conservative treatments are insufficient, surgical options may be considered. This type of surgery allows for a more comprehensive view and treatment of the joint structure. The appliance worn is converted into a surgical splint and adjusted every month for about 6 months. This allows for healing from the surgery where the disc was replaced on top of the condyle (Disc plication surgery) or if severely damaged then the disc will be removed (meniscectomy).
Additionally, some patients may benefit from regenerative medicine techniques, such as platelet-rich plasma (PRP) injections, which aim to promote healing and reduce inflammation in the joint. These treatments are often considered experimental and should be discussed thoroughly with a healthcare provider.
Ultimately, the choice between conservative and surgical treatments should be made in consultation with a TMJ specialist, who can tailor the treatment plan to the individual’s specific condition and needs.
Preventing TMJ Disc Perforation
Preventing TMJ disc perforation involves proactive measures to minimize risk factors and maintain joint health. Stress management is essential, as reducing stress can help prevent teeth grinding and clenching, which place excessive pressure on the TMJ. For those who grind their teeth at night, wearing a mouthguard while sleeping can provide a protective barrier that reduces the impact on the joint. Keep in mind this is only while you wear it. It should be understood that a nightguard can only be worn if the patient is cleared for obstructive sleep apnea and underlying TMJ disorder. Be sure you see a real TMJ specialist who understands the implications of the guard. Regular dental check-ups are important for identifying and addressing issues like bruxism early on.
Maintaining good posture, especially while working at a desk or using electronic devices, can also reduce strain on the jaw and neck muscles. Being aware of your jaw movements and avoiding habits like chewing gum or biting nails can help reduce unnecessary stress on the TMJ. If you participate in contact sports or activities that risk facial injuries, wearing appropriate protective gear can help prevent trauma to the jaw.
Dietary choices can also play a role in prevention. Consuming softer foods and avoiding those that require extensive chewing can help minimize strain on the TMJ. Additionally, incorporating jaw exercises as recommended by a healthcare provider can strengthen the muscles around the joint, promoting better support and function.
By adopting these preventive measures, individuals can reduce the risk of developing a perforated TMJ disc and maintain overall joint health. Regular follow-ups with a TMJ provider ensure that the condition is monitored closely, and treatment plans can be adjusted as needed. Using pain management techniques can significantly improve daily comfort and quality of life.
By adopting these strategies and remaining vigilant about their condition, individuals can better manage their symptoms and lead a more comfortable, active life.
