Grasping TMJ Disc Perforation
TMJ articular disc perforation occurs when the disc within the temporomandibular joint sustains a tear or hole. This disc is essential for cushioning the bones of the joint and ensuring smooth, pain-free movement of the jaw. A perforation disrupts this function, leading to discomfort and mechanical problems with jaw movement. People with this condition may notice an array of symptoms that affect their daily lives, making it challenging to chew, speak or even yawn comfortably.
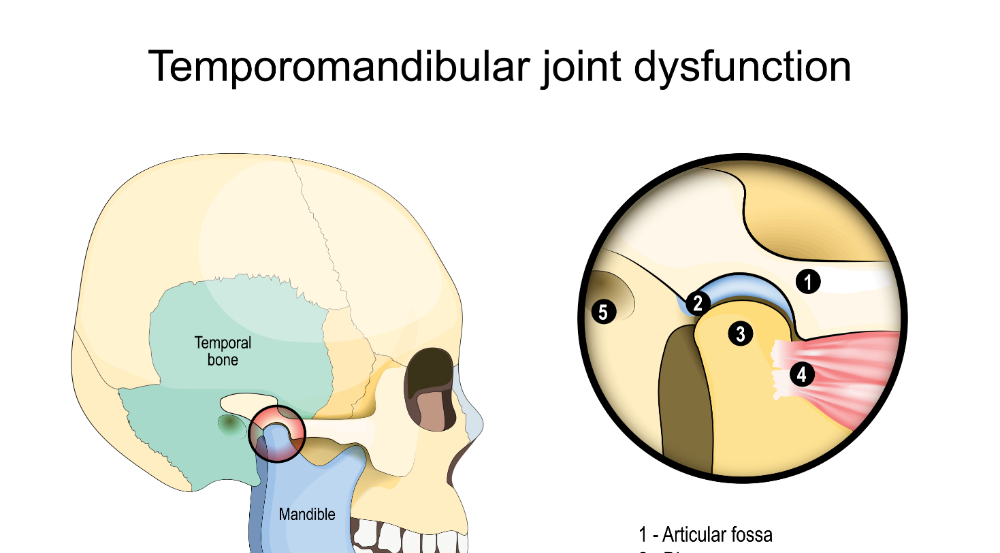
The temporomandibular joint itself is a unique and intricate system. It connects the lower jaw (mandible) to the skull, allowing for complex movements required for chewing, talking and other activities. The articular disc within this joint is made of fibrocartilage and is designed to withstand significant stress and pressure. However, factors like trauma, bruxism and arthritis can cause this disc to weaken and eventually perforate.
Understanding what leads to TMJ disc perforation is crucial for effective management and prevention. Traumatic events such as sports injuries, car accidents or any direct impact to the jaw can cause immediate damage to the disc. On the other hand, chronic conditions like bruxism involve repetitive grinding or clenching of the teeth, which exerts constant pressure on the disc, leading to gradual wear and tear. Additionally, arthritis can degrade the joint structures over time, making the disc more prone to perforation.
Recognizing the importance of this disc and its function within the TMJ helps to appreciate the impact of perforation. It is not merely a structural issue but one that can significantly impair the quality of life. For instance, individuals with this condition may experience severe discomfort, mechanical restrictions in jaw movement and associated symptoms like headaches or earaches.
The anatomy and functionality of the TMJ and its components, particularly the articular disc, underline the necessity of addressing any damage promptly. Proper diagnosis and tailored treatment plans can help mitigate the effects of a perforated disc, allowing individuals to regain normal jaw function and alleviate pain.
Causes Behind TMJ Disc Perforation
Various factors can contribute to the development of TMJ disc perforation. Trauma to the jaw is one primary cause. This can result from incidents such as sports injuries, falls or car accidents where direct impact is sustained by the jaw. Such traumatic events can lead to immediate damage to the disc, disrupting its function and causing a perforation.
Chronic conditions also play a significant role. Bruxism, or the habitual grinding and clenching of teeth, exerts continuous pressure on the TMJ disc. Over time, this repeated stress can wear down the disc, eventually leading to perforation. People who experience high levels of stress or anxiety are more likely to develop bruxism, increasing their risk for TMJ disc damage.
Arthritis is another notable contributor. Both osteoarthritis and rheumatoid arthritis can degrade the cartilage and other structures within the TMJ. This degradation weakens the joint and makes the disc more prone to perforation. Age-related wear and tear associated with osteoarthritis can cause the disc to deteriorate gradually, while the inflammatory processes in rheumatoid arthritis can accelerate joint damage.
Genetic predisposition may also influence the likelihood of developing TMJ disc perforation. Individuals with a family history of TMJ disorders or connective tissue diseases might be more susceptible to disc damage. Additionally, certain anatomical abnormalities in the jaw or TMJ can predispose individuals to this condition.
Habits and lifestyle choices can further exacerbate the risk. Repetitive behaviors such as chewing gum excessively, biting nails or using the teeth to open packages can strain the TMJ. Occupational hazards, like jobs requiring prolonged speaking or jaw movements, can also contribute to disc wear.
Understanding these causes is crucial for preventing TMJ disc perforation. By identifying and mitigating risk factors, individuals can take steps to protect their TMJ health and reduce the likelihood of experiencing this painful and debilitating condition.
Symptoms and Diagnosis
Jaw pain is one of the most common signs of TMJ disc perforation. People with this condition often report discomfort that can range from mild to severe. This pain can be persistent or intermittent, and it may worsen with jaw movement. In addition to pain, individuals might notice clicking or popping sounds when they open or close their mouths. These sounds occur due to the irregular movement of the damaged disc within the joint.
Difficulty in opening or closing the mouth is another key symptom. Some individuals might experience a limited range of motion, making it hard to perform everyday activities like eating or speaking. This restriction can vary from person to person and can be quite frustrating. Headaches are also frequently associated with TMJ disc perforation. These headaches can range from tension-type headaches to more severe migraines and can significantly impact daily life.
To diagnose TMJ disc perforation, healthcare professionals often turn to imaging techniques. MRI (Magnetic Resonance Imaging) is a common tool used to get a detailed look at the soft tissues in the joint, including the articular disc. CT (Computed Tomography) scans can also provide valuable information by offering a clear picture of the joint’s bony structures. These imaging methods help in confirming the presence of a perforation and assessing the extent of the damage.
Clinical examination is another crucial component of the diagnostic process. A healthcare provider may palpate the jaw area to check for tenderness, listen for abnormal sounds during jaw movement, and assess the range of motion. These steps, combined with patient history and reported symptoms, aid in forming a comprehensive diagnosis.
In a study by Johansson et al., it was found that pain from TMJ affected 6.7% of males and 12.4% of females, highlighting the importance of addressing these symptoms promptly (Johansson et al., 2002).
Early and accurate diagnosis is vital for the effective management of TMJ disc perforation. The combination of patient-reported symptoms, clinical evaluation and advanced imaging techniques provides a robust framework for identifying and addressing this condition. Perhaps the best imaging to confirm a perforation of the disc is an MRI of the TM joints. For some reason, MRI imaging of the TM joints is somewhat controversial. I believe this is because so few doctors actually order the imaging, or so few radiologists are familiar with reading this MRI. It takes a lot of experience to understand how to read this imaging.
Treatment Options
To treat TMJ articular disc perforation, both conservative and surgical methods are available. Conservative management often involves physical therapy to improve jaw function and reduce pain. Physical therapists may guide patients through exercises designed to strengthen the jaw muscles and improve mobility. Medications can also play a role in alleviating symptoms. Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly prescribed to manage pain and inflammation associated with TMJ disorders.
Another conservative approach is the use of an orthotic, especially for those who suffer from bruxism. These devices help to minimize teeth grinding and clenching, which can further damage the TMJ disc. Orthotics are custom-made to fit an individual’s teeth and provide optimal protection. They are made to fit to the lower teeth and MUST be worn 24/7 so that the condyle does not further damage an already compromised disc. Within our practice, for those who want to finish with this lower appliance, and we have determined the correct height of the back teeth, then we can finish with orthodontics (Spark Aligners). Many patients prefer this to traditional braces.
In more severe cases, surgical interventions may be necessary. Arthrocentesis is one less invasive surgical option where the joint is flushed with fluid to remove debris and reduce inflammation. For more significant damage, open joint surgery might be required. This procedure allows surgeons to repair or remove the damaged disc. It must be understood that arthrocentesis, although more conservative, does nothing to correct the damaged disc, it only might help reduce the symptoms and make them more manageable.
Joint realignment procedures are another surgical option, aimed at correcting any misalignment that contributes to the wear and tear of the disc. Minimally invasive techniques such as arthroscopy can be employed to perform these corrections with smaller incisions, leading to quicker recovery times. Again, only an open joint surgery can remove the actual disc.
The choice between conservative and surgical treatment depends on the severity of the condition and individual circumstances. Consulting with healthcare professionals specializing in TMJ disorders is crucial for an accurate diagnosis and personalized treatment plan. By tailoring the approach to the specific needs and conditions of the patient, effective management of TMJ articular disc perforation can be achieved.
Recovery and Management
Recovery from TMJ disc perforation treatment requires dedication to a structured care plan to achieve optimal healing and prevent future issues. After either conservative or surgical treatment, patients should closely follow their healthcare provider’s recommendations, which might include attending scheduled follow-up appointments to monitor progress and make necessary adjustments to the treatment plan.
Massage therapy and sometimes physical therapy play a significant role in the recovery process. It can help restore normal jaw function and reduce discomfort. Patients are often provided with exercises tailored to their specific needs to strengthen the jaw muscles and enhance mobility. These exercises should be performed consistently and correctly to maximize their benefits.
Medications may continue to be part of the recovery process, especially if there is ongoing pain or inflammation. It is essential to use these medications as directed and report any side effects or concerns to the healthcare provider promptly.
Lifestyle modifications are equally important in managing recovery. Incorporating stress management techniques can help reduce habits like teeth clenching and grinding, which can exacerbate TMJ issues. Practices such as meditation, deep-breathing exercises and yoga can be beneficial in managing stress levels. Additionally, a soft diet can help minimize strain on the jaw during the healing process. Foods like mashed potatoes, yogurt and smoothies are good options that do not require extensive chewing.
Good posture, particularly during activities that involve prolonged speaking or jaw movements, can also aid in reducing stress on the TMJ. Avoiding habits such as chewing gum or biting nails will further protect the joint from unnecessary wear.
By diligently following these recovery and management strategies, individuals can significantly improve their chances of a successful outcome and reduce the risk of future complications associated with TMJ articular disc perforation.
If you currently struggle with TMJ issues and want to learn more about TMJ treatments in Falls Church, Virginia, we are here to help. Dr. Jeffrey Brown and our team at Sleep & TMJ Therapy can help you find the relief you need. Please call 703-821-1103 to learn more or schedule a consultation with Dr. Brown.
